Clair360 an affordable solution to accurately calculate the risk adjustment factor and identify quality gaps


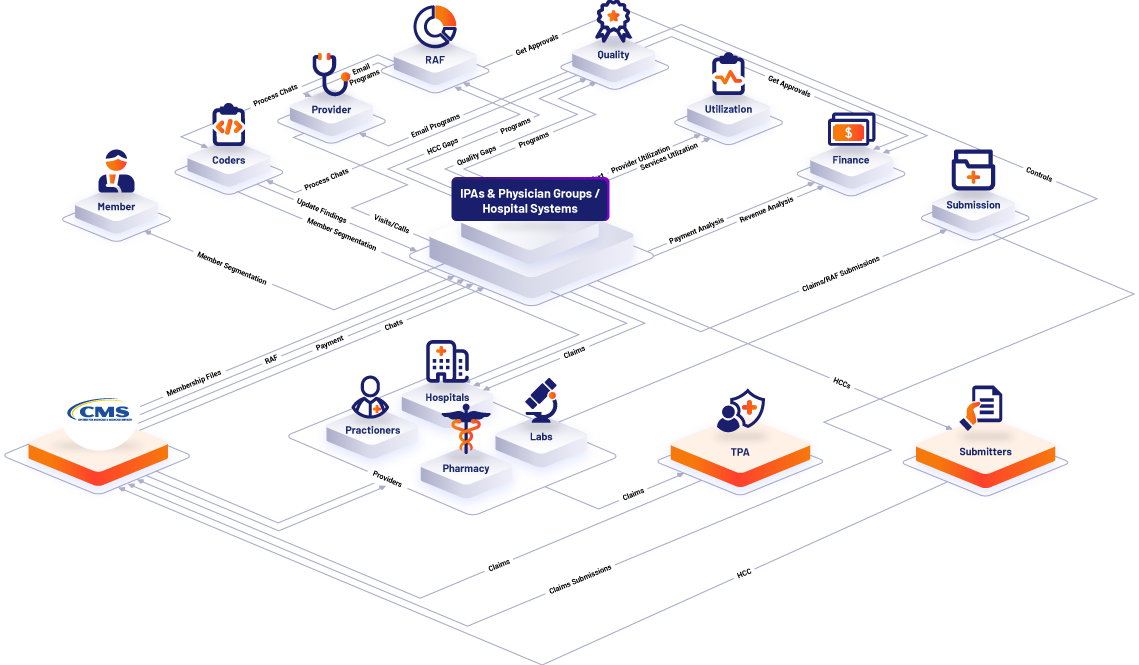
Clair360™, an interactive, fully integrated, and AI-based platform with multi-module solutions, that identifies risk adjustment and quality issues and communicates in real time to all internal and external stakeholders how to resolve them. Clair360™ plugs into the existing IT infrastructure of Medicare Advantage plans, provider groups and hospital/health systems via APIs.

No Investment, No specialized IT talent required.

Internal and external parties in real time-Improved communication and outcomes.

Improved health outcomes to get more members

Affordable and within the capabilities of current staff with AWS-Hosted data encryption.

Clair360™ Plugs your organization with all your healthcare organization partners.

Scalable from the smallest to the Largest Payer and Provider Organizations.
Clair360™

This member-centric module provides 360° insight about your members. It compares current demographic and health status to historical statuses and predicts future status. This results in better membership management by closing gaps in the member’s healthcare and quality measures.

This module includes a clinical coding tool that has automated NLP-based charts and data review processes which allows organizations to capture various data like diagnosis codes, procedure codes, quality measures, and much more.

This module focuses on providers to measure and enhance the quality, completeness, and efficiency of the services provided to the patients. It provides in-depth statistics and analytics to highlight any provider’s gaps and issues and how to resolve it.

The heart of the Risk Adjustment program is the RAF360. The focus is on membership RAF: Defining the current RAF, past RAF, future RAF – what it will be, and what it should be. Our goal is to identify all gaps and predict possible gaps to capture by using complex and validated analytical models.

This module identifies the current quality measures status, identifies the gaps, and provides possible ways to close them which will help improving quality performance metrics. Self-Managed AI-based module that allows you to update your measures status as frequently as needed.

This module provides a 360° view of claims. It allows users to slice and dice the complex claims data to provide answers to business questions like utilization, costs, and statistics easily. In addition, it utilizes claims data to get an accurate PMPM and to identify possible ways to reduce it

This module focuses on cash flow and the RA payment models and processes to help organizations identify what likely payment when they should receive payment, and identify any gaps in payments.

This module provides a complete picture of submissions. It reconciles what has been submitted with what should have been submitted. Also, it finds the gaps, rejections, and other issues in the submission process then it creates files to submit missing data.

This built in fully integrated task management module enhanced managing, communication, tracking and reporting all projects and tasks related to programs and process within the Clair360™. It provides an easy and interactive way to create, assign and track tasks to team members and providers.